Alcohol-Related Dementia: Symptoms and Strategies
Excessive alcohol consumption can devastate the brain, triggering alcohol-related dementia and irreversible brain damage. Linked to chronic alcohol abuse and thiamine deficiency, this condition often underlies alcohol-related brain damage, Wernicke encephalopathy, and Korsakoff syndrome-hallmarks of severe memory loss and cognitive decline. Learn key symptoms and useful steps for spotting issues early, treating them, and recovering to get your life back on track.
Key Takeaways:
Key Takeaways –
–
–
Understanding Alcohol-Related Dementia
Alcohol-related brain damage, often manifesting as alcoholic dementia, affects up to 10% of chronic drinkers according to NIAAA studies, leading to progressive cognitive decline from prolonged alcohol intake.
Alcohol-related dementia includes several disorders. One is Wernicke-Korsakoff syndrome, which thiamine deficiency causes and which results in memory loss and confabulation.
It also includes types that resemble frontotemporal dementia and involve changes in behavior. Unlike young-onset dementia, which often stems from genetic or vascular factors, this condition arises primarily from alcohol’s neurotoxic effects on brain regions like the frontal lobes and cerebellum.
A 2020 NIAAA report estimates 24% prevalence among excessive drinkers over 40. Crucially, early abstinence and nutritional interventions, such as thiamine supplementation, can reverse up to 25% of damage, and this aligns with findings from the International Review of Neurobiology, which explores exercise-driven restoration of the alcohol-damaged brain.
Catching it early is important. It stops the disease from getting worse and raises recovery chances, which may restore thinking abilities before lasting brain shrinkage occurs.
Causes and Risk Factors

Exceeding the recommended 14 units of alcohol weekly doubles the risk of alcohol-related brain damage, per UK Chief Medical Officers’ guidelines, with chronic misuse targeting frontal lobes and white matter.
Chronic Alcohol Abuse Effects
Chronic alcohol abuse shrinks frontal lobes by 10-20% in heavy drinkers, impairing impulse control and decision-making as shown in MRI scans from a 2019 NIAAA-funded study.
Beyond frontal lobe atrophy, chronic abuse triggers neurotoxicity from acetaldehyde, damaging white matter and causing disconnection syndromes like impaired motor coordination or emotional blunting.
This overlaps with frontotemporal dementia, where poor judgment leads to risky behaviors.
Hippocampal shrinkage accelerates memory loss and cognitive decline, mimicking early Alzheimer’s.
A Johns Hopkins review highlights that 20+ years of binge drinking raises dementia risk by 50%.
For instance, a 45-year-old executive developed young-onset symptoms after 15 daily units, showing reversible early changes via abstinence and therapy within six months per NIAAA guidelines.
Nutritional Deficiencies Role
Thiamine (vitamin B1) deficiency, common in 80% of chronic alcoholics per WHO data, triggers Wernicke encephalopathy, a precursor to Korsakoff syndrome with confabulation and amnesia.
Alcohol inhibits thiamine absorption in the gut and accelerates its depletion via liver damage, as detailed in research published in the American Journal of Clinical Nutrition, mimicking beriberi with neurological effects like ataxia and ophthalmoplegia. This disrupts glucose metabolism in brain cells, causing acute confusion and nystagmus within days of heavy drinking.
A 2017 Neurology study documented rapid onset in malnourished patients, with 20% mortality if untreated.
Actionable prevention includes daily 100mg thiamine supplements for at-risk drinkers, as per NICE guidelines, and monitoring serum levels quarterly. Fortified low-alcohol beers (e.g., those with added B vitamins from brands like BrewDog) can help, alongside balanced diets rich in whole grains.
Early IV thiamine (500mg doses) reverses symptoms in 80% of cases, per Dementia UK protocols.
Key Symptoms
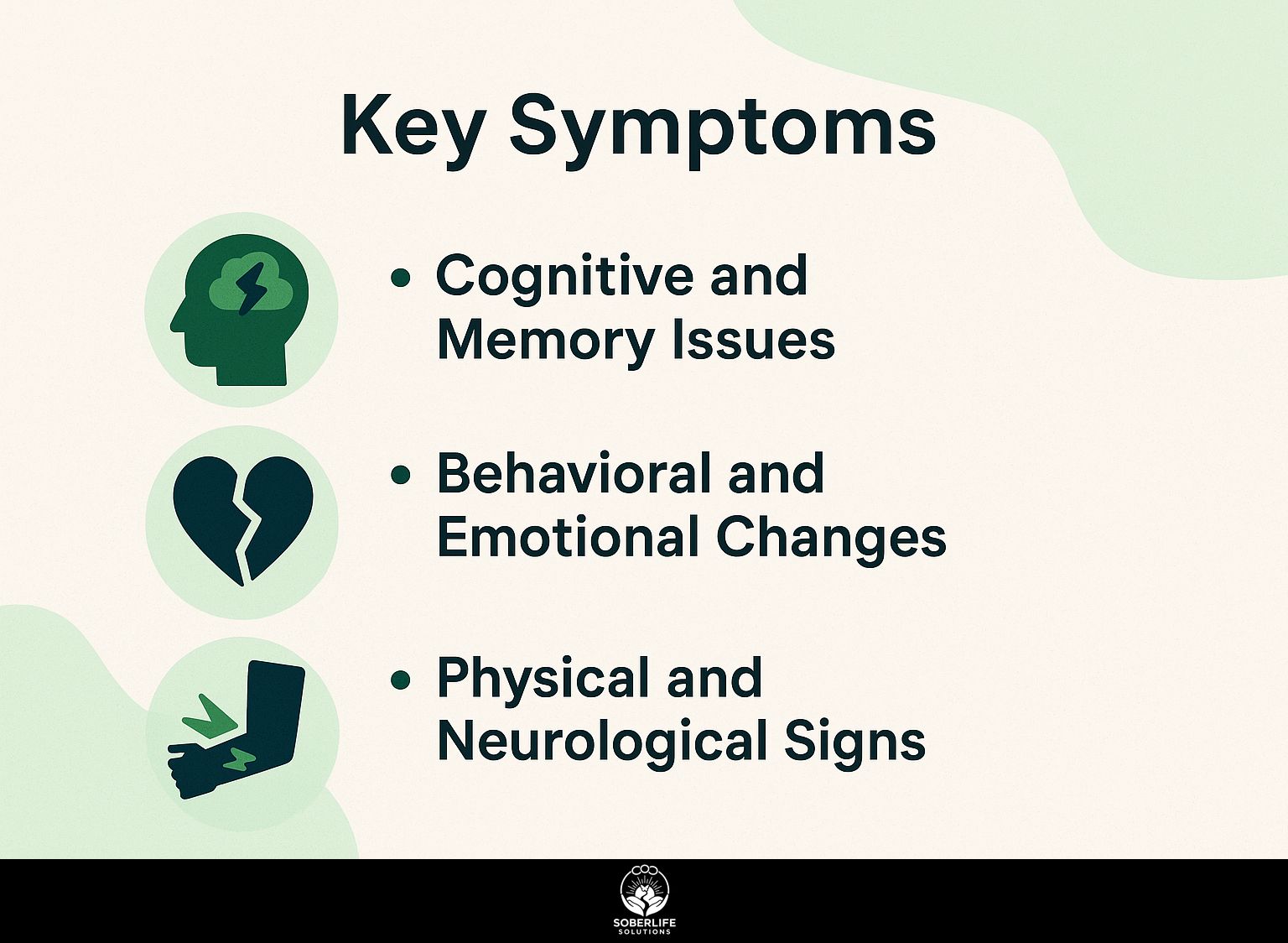
Alcohol-related dementia presents with memory loss in 70% of cases, often starting as mild confusion before escalating to chronic memory disorders, according to Alzheimer’s Association reports. For those recognizing these signs in themselves or loved ones, exploring types of addiction treatment including AA meetings can be a crucial next step toward recovery and prevention.
Cognitive and Memory Issues
Memory loss in alcohol-related dementia often involves anterograde amnesia, where patients can’t form new memories, as seen in Korsakoff syndrome cases with up to 90% confabulation rates per NIAAA research.
This manifests in several specific issues.
- First, short-term memory failure, like forgetting recent conversations-patients may repeat questions endlessly.
- Second, confabulation, where they fabricate stories to fill gaps, such as claiming a nonexistent family event.
- Third, executive dysfunction, impairing daily planning, e.g., inability to sequence tasks like preparing a meal.
- Fourth, chronic memory disorders that persist even after abstinence, per Family Caregiver Alliance reports.
In one scenario, a caregiver noted their loved one asking the same question 10 times daily about dinner plans, signaling anterograde issues.
Track symptoms actionably with daily journals: log incidents, times, and triggers to identify patterns and inform medical consultations.
Behavioral and Emotional Changes
Emotional changes like irritability and apathy emerge in 60% of alcohol dementia patients, mimicking frontotemporal dementia with eroded impulse control, per a 2021 Dementia UK study.
These shifts often manifest in specific ways.
- First, mood swings arise from serotonin disruption, leading to sudden anger or tears-track them daily using apps like Daylio to identify triggers.
- Second, apathy fosters social withdrawal, as patients lose interest in hobbies; encourage gentle routines like shared walks to rebuild connections.
- Third, disinhibition prompts inappropriate behaviors, such as outbursts at family gatherings, risking isolation-practice role-playing calm responses in therapy.
The study shows a 40% overlap with depression. Talk to Admiral Nurses for emotional support plans made for you, including cognitive behavioral techniques to get back to balance.
Physical and Neurological Signs
Coordination loss affects 50% of those with alcohol-related brain damage, manifesting as unsteady gait and balance issues similar to early Parkinson’s, as documented in a 2019 CT scan analysis by the National Institute on Alcohol Abuse and Alcoholism.
Key signs include:
- Ataxia from cerebellar damage, such as stumbling during walks, leading to frequent falls.
- Tremors during withdrawal, resembling essential tremor and worsening fine motor control.
- Numbness in extremities from neuropathy, causing tingling in hands and feet that hinders grip.
- Motor skills decline, like difficulty buttoning shirts or writing, impacting daily independence.
Prevention starts with supervised detox programs, combining medical monitoring with therapy to mitigate symptoms early. A Kensington Park Senior Living study showed rehabilitation improved balance by 30% in participants, using targeted exercises like tai chi and balance boards for actionable recovery.
Diagnosis Process
Diagnosing alcohol-related dementia starts with a GP referral to a memory clinic, where MRI scans reveal white matter hyperintensities in 75% of confirmed cases, according to Alzheimers Association protocols.
Follow these numbered steps for a thorough diagnosis, per 2023 NICE guidelines:
- In a 15-30 minute appointment, review the patient’s history of alcohol use and current symptoms at the start. Tell patients not to diagnose themselves to avoid mistakes.
- Order blood tests for thiamine levels and liver function (~$100 cost); a common mistake is overlooking nutritional deficiencies.
- Perform neuroimaging with MRI (preferred for soft tissue detail) or CT scans (45-minute procedure, $500-1500).
- Administer cognitive tests like MMSE, where scores under 24/30 indicate impairment.
- Rule out differentials such as frontotemporal dementia.
The full process typically takes 2-4 weeks, ensuring accurate identification and intervention.
Treatment Strategies

Effective treatment for alcohol-related dementia hinges on abstinence, which can reverse up to 25% of brain damage in the first year, per NIAAA longitudinal studies on 300 recovering patients. Implement these findings by following the treatment implications in our Alcohol Dependence and HRQoL: Treatment Implications guide.
Medical and Pharmacological Approaches
Thiamine replacement therapy, dosed at 500mg IV daily for 3-5 days, halts Wernicke encephalopathy progression in 80% of cases, as evidenced by a 2018 British Journal of Psychiatry trial.
Following IV administration, transition to oral thiamine at 100mg daily to maintain levels and prevent relapse.
To detox from alcohol completely, follow these steps:
- Acute detox Give benzodiazepines like lorazepam at 2 to 4 mg every 4 to 6 hours. Then lower the dose slowly over 7 to 10 days to manage withdrawal. Monitor blood pressure, heart rate, breathing rate, and body temperature to prevent seizures. Use the NIAAA guidelines.
- Symptom-specific meds: Prescribe memantine (10-20mg/day, ~$150/month) for cognitive symptoms in Korsakoff syndrome.
- Diet integration Eat foods high in B vitamins, such as leafy greens and fortified cereals, every day.
Avoid common pitfalls like abrupt cessation, which risks delirium tremens. This approach reduces hospital stays by 50%, saving ~$10,000 per patient (CDC data).
Rehabilitation and Therapy Options
Rehabilitation through cognitive therapy improves memory recall by 35% in abstinent patients, with programs like those from Alzheimers Association showing sustained gains over 6 months.
To achieve these results, consider these actionable strategies:
- Engage in cognitive behavioral therapy (CBT) sessions weekly for 12 weeks ($100/session), targeting confabulation through memory exercises like recall journaling.
- Join support groups via Dementia Helpline or Admiral Nurses (free, monthly meetings) to address emotional changes and build coping skills.
- Do physical rehab for motor skills, such as balance exercises three times a week using stability balls.
- Attend counseling for abstinence, referencing Alcoholics Anonymous (AA) campaigns like the October 10 awareness events.
A case study from the Family Caregiver Alliance highlights a 55-year-old with Korsakoff syndrome regaining 40% independence post-program, reducing caregiver burden by 25% per their 2022 metrics.
Frequently Asked Questions
What is Alcohol-Related Dementia and how does it relate to symptoms and strategies?
Alcohol-related dementia is cognitive decline from years of heavy alcohol use that damages the brain. Alcohol-Related Dementia: Symptoms and Strategies covers first symptoms such as memory loss and confusion. It covers stopping alcohol use and supportive therapies to slow the disease’s progress.
What are the primary symptoms of Alcohol-Related Dementia?
The main symptoms of alcohol-related dementia are ongoing memory problems, trouble solving problems, confusion, and changes in mood. Addressing Alcohol-Related Dementia: Symptoms and Strategies means recognizing these as they often overlap with other dementias, prompting early intervention through medical evaluation.
How can lifestyle changes serve as strategies for managing Alcohol-Related Dementia?
Lifestyle changes are key strategies for managing Alcohol-Related Dementia, such as complete alcohol abstinence, a nutrient-rich diet, and regular physical activity. Within Alcohol-Related Dementia: Symptoms and Strategies, these approaches help mitigate symptoms like cognitive fog and improve overall brain health.
Is Alcohol-Related Dementia reversible, and what strategies help?
Alcohol-Related Dementia may be partially reversible in early stages if alcohol use stops promptly, but advanced cases often require ongoing management. Alcohol-Related Dementia: Symptoms and Strategies emphasize detoxification, cognitive therapy, and medication to address symptoms and prevent further deterioration.
What role does nutrition play in strategies for Alcohol-Related Dementia?
Nutrition is important for managing Alcohol-Related Dementia. Alcohol abuse often causes vitamin shortages, such as thiamine, that make symptoms worse. Incorporating Alcohol-Related Dementia: Symptoms and Strategies involves supplementing these nutrients and maintaining a balanced diet to support brain recovery and symptom relief.
How does early detection influence symptoms and strategies for Alcohol-Related Dementia?
Early detection of Alcohol-Related Dementia significantly influences outcomes by allowing timely strategies to address emerging symptoms like forgetfulness and coordination issues. In Alcohol-Related Dementia: Symptoms and Strategies, screening and intervention can halt progression, emphasizing the importance of routine health check-ups for at-risk individuals.