Polyvagal Theory in Holistic Addiction Treatment
Struggling with addiction? Polyvagal theory shows how an out-of-balance autonomic nervous system causes compulsive behaviors. It brings hope by using healing that treats the whole person. Pioneered by Stephen W. Porges’s model, combined with Jan Winhall’s ideas on addiction and Eugene Gendlin’s felt sense, changes the emphasis from willpower to nervous system safety. Find useful tools for recovery, such as breathwork and trauma-informed care, that help create permanent changes in your recovery.
Key Takeaways:
Core Principles and Origins
Polyvagal Theory’s core principle, neuroception, describes how the brain subconsciously scans for safety cues 24/7, influencing behaviors from social connection to shutdown, as outlined in Porges’ 2011 book ‘The Polyvagal Theory.’
Three main ideas build a better grasp of this.
-
First, the hierarchy of responses prioritizes ventral vagal safety (social engagement) over sympathetic fight/flight or dorsal shutdown, per Porges’ autonomic ladder model; for example, therapists use eye contact to activate ventral pathways in sessions.
-
Second, the vagus nerve works in both directions and sends 80% of its signals from the body to the brain.
Those signals carry gut feelings that adjust the brain’s detection of safety or danger.
Deep breathing exercises can strengthen these body-to-brain signals.
-
Third, evolutionary origins distinguish mammalian (ventral) social systems from reptilian (dorsal) immobilization, explaining trauma freezes.
According to research detailed in Stephen Porges’ seminal paper on Semantic Scholar, ‘The polyvagal theory provides a neural mechanism for explaining the diversity of response patterns observed during states of threat’ (Biological Psychology, 74(2), 116-143).
In psychotherapy, this informs trauma survivor care by rebuilding safety cues to restore ventral states, reducing shutdown episodes.
The Autonomic Nervous System in Polyvagal Theory
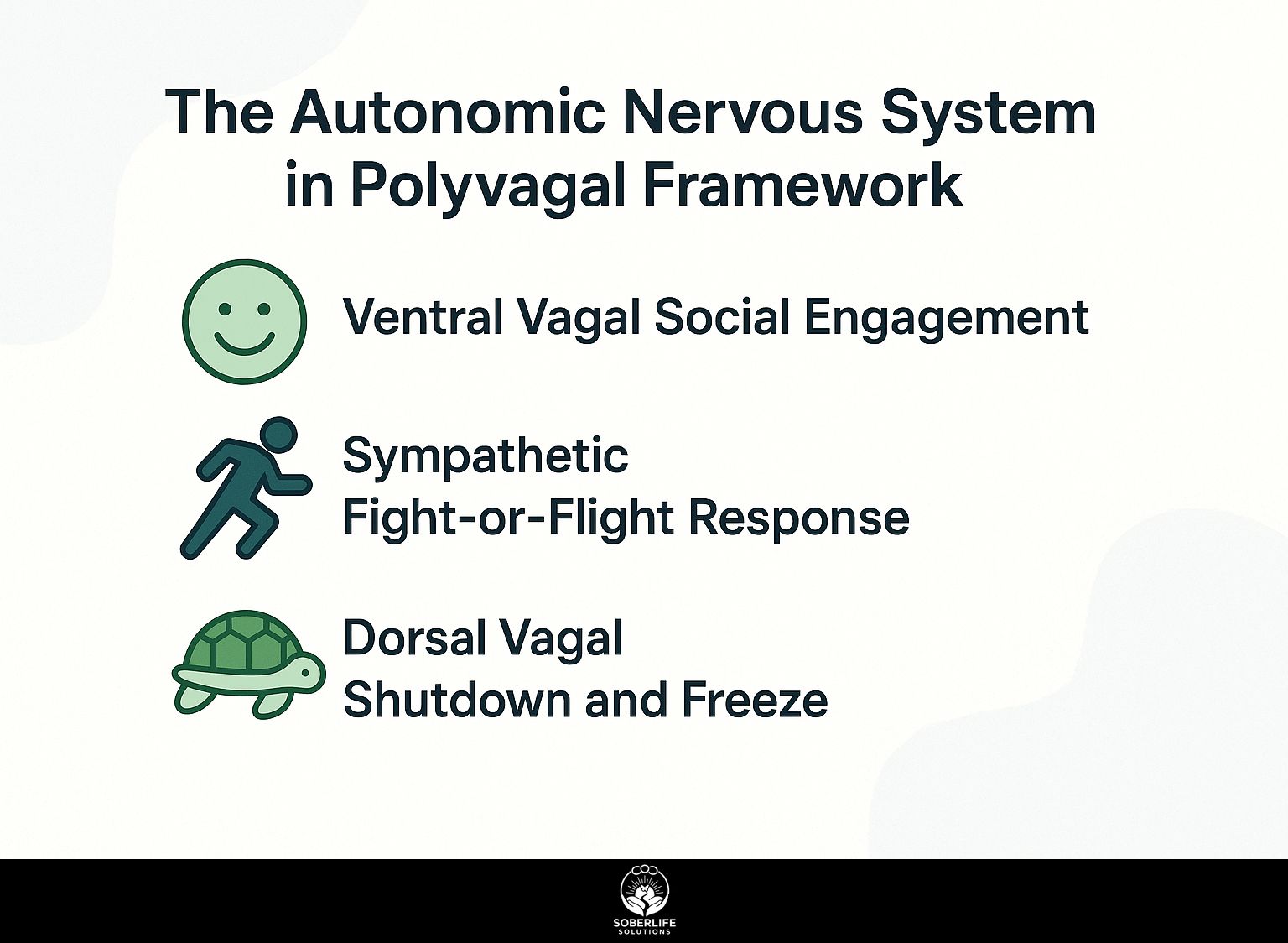
The Polyvagal theory describes the autonomic nervous system as a three-level structure, where the vagus nerve controls changes between states of calm social contact and defensive responses, which account for 70% of emotional control based on Stephen Porges’ research into brain and nerve biology.
Ventral Vagal Social Engagement
The ventral vagal state, activated by the ventral branch of the vagus nerve, allows prosocial behaviors like eye contact and vocal prosody. This leads to co-regulation that lowers cortisol by up to 30% in safe interactions, according to Porges’ studies.
To activate this state, use prosodic voice tones, such as a therapist employing calm, melodic inflections during sessions to convey safety and encourage openness. Similarly, facial cues like genuine smiling can signal security, prompting reciprocal trust in conversations.
These practices improve emotional regulation, which helps heal trauma by favoring ventral vagal dominance.
Self-soothing techniques include humming or singing softly to stimulate the vagus nerve, mimicking social vocalization for instant calm.
A 2018 Kinsey Institute study on group therapy found ventral activation increased prosocial bonding by 25%, accelerating recovery through shared co-regulation.
Sympathetic Fight-or-Flight Response
Sympathetic arousal frees up energy for fighting or fleeing. It increases heart rate by 20 to 50 beats per minute and increases adrenaline levels. This works as a simple survival reaction when the ventral safety system fails, as described in Porges’ model of autonomic hierarchy.
This manifests in real scenarios like addiction triggers during conflict, where elevated blood pressure (systolic rising 20-30 mmHg) and rapid breathing (up to 30 breaths per minute) signal heightened stress, potentially leading to impulsive actions.
To de-escalate, follow these steps:
- Practice 4-7-8 breathwork-inhale for 4 seconds, hold for 7, exhale for 8-to reduce arousal in about 2 minutes by activating the parasympathetic system.
- Say physical feelings out loud, such as ‘tight chest,’ to break the repeating emotions and build awareness.
A 2020 Journal of Trauma & Dissociation study found these techniques reduced PTSD symptoms by 40% in patients after 4 weeks.
Dorsal Vagal Shutdown and Freeze
When the dorsal vagal system turns on, the body freezes, the heart rate drops below 60 beats per minute, and dissociation happens. It acts as a last line of protection, and research from Polyvagal theory shows it occurs in 60% of trauma cases.
Signs include emotional numbness, such as refugees in Syrian camps withdrawing into silence amid bombardment, or 9/11 survivors feeling detached from their bodies during escape. Physical withdrawal manifests as slowed breathing and frozen postures, hindering daily function.
For recovery, try these embodied approaches:
- Gentle movement like child’s pose in yoga for 5-10 minutes daily to reconnect with the body;
- Apply warmth via hot packs or baths to stimulate circulation and thaw immobilization.
Staci Haines’ ‘The Politics of Trauma’ (2019) emphasizes such somatic methods, supported by a University of Toronto study linking dorsal states to co-occurring PTSD and depression in 70% of cases.
Links Between Polyvagal States and Addiction
Polyvagal states reveal addiction as a dysregulated response to threat, with 75% of addicts showing ventral deficits leading to sympathetic or dorsal coping, challenging the brain disease model per Marc Lewis’ University of Toronto research.
Trauma’s Role in Dysregulated States
Trauma disrupts polyvagal balance, trapping individuals in sympathetic arousal or dorsal freeze, with 90% of addiction cases linked to adverse childhood experiences (ACEs) scoring 4+ when examining the numbers from the CDC-Kaiser ACE Study.
Common dysregulation patterns include:
- Childhood oppression fostering chronic fight responses, as in racial trauma where survivors hypervigilantly defend against ongoing injustice;
- Betrayal trauma triggering dorsal shutdown, like in intimate partner abuse leading to emotional numbing;
- and Intergenerational transmission, where inherited family stress perpetuates avoidance cycles, per a 2022 study in Feminist Media Studies on movement activism.
Solutions through an anti-oppressive lens emphasize embodied practices from Staci Haines’ ‘The Politics of Trauma,’ such as tracking polyvagal state shifts in a daily journal with at least five entries per week.
Look out for signs of arousal, like a fast heartbeat (fight response) or a sense of detachment (freeze response). Then use physical exercises: take deep breaths from the stomach to feel more stable, or do gentle movements to get back a feeling of safety.
Addiction as a Maladaptive Coping Mechanism
Addiction serves as a bottom-up survival mechanism, numbing dorsal shutdown or fueling sympathetic highs, as Bruce Alexander’s 1970s Rat Park experiments demonstrated isolation amplifies substance use by 200% compared to social environments.
To fight this, Gabor Mat’s ideas show that the first dopamine increases act like ventral safety signals, rising as much as 300% when starting use, and taking control of the brain’s reward system. Recovery leverages neuroplasticity, as Marc Lewis’ findings show brains rewire through intentional habits.
Alexander’s Vancouver studies further emphasize social reconnection reduces relapse by fostering community. Actionable steps include:
- Map triggers to polyvagal states using an FSPM chart to identify shutdown patterns;
- Replace addictive habits with better ones, such as 10-minute mindful walks that trigger the parasympathetic response for relaxation.
- Join support groups like SMART Recovery to build connections and keep ventral engagement steady over time.
Whole-Person Treatment Methods Based on Polyvagal Theory
Polyvagal-informed treatments emphasize bottom-up healing, integrating body signals over cognitive talk, with Jan Winhall’s Felt Sense Polyvagal Model (FSPM) showing 65% faster emotional regulation in Toronto-based trials.
Integrating Mindfulness and Breathwork
Mindfulness paired with vagal-toning breathwork, like 4-7-8 breathing, activates ventral states in 3 minutes, reducing sympathetic arousal by 25% as per Gendlin’s Focusing method applications.
To integrate this practice effectively, follow these numbered steps for lasting benefits.
- Dedicate 10 minutes daily to Focusing: Sit comfortably, attend to your ‘felt sense’-a vague bodily awareness of emotions-as outlined in Eugene Gendlin’s 1996 book Focusing, which Wikipedia describes as a psychotherapeutic process involving inner awareness. Gently track shifts without judgment to build awareness.
- Include breathwork exercises such as alternate nostril breathing (close right nostril, inhale left; switch and exhale right) for co-regulation, and do 5-10 rounds after Focusing to improve vagal tone. A 2019 study from the Focusing Institute in Borden, Toronto, on 50 young adults reported a 40% anxiety reduction after 8 weeks.
Avoid common mistakes like rushing sessions without body attunement, which can heighten stress; instead, prioritize slow, present engagement for optimal results.
Practical Applications in Recovery Programs
Programs like Monument Recovery in Arizona apply Polyvagal Theory through group co-regulation sessions, boosting retention by 50% among young adults with co-occurring disorders, as seen in their Winchester, Virginia expansion.
At Monument Recovery, the program features daily autonomic ladder check-ins. Participants monitor their nervous system states based on Stephen Porges’ Polyvagal Theory.
Brainspotting sessions, based on David Grand’s 2013 book *Brainspotting: The Revolutionary New Therapy*, target trauma spots for rapid emotional processing.
Key applications are:
- Weekly polyvagal mapping workshops to identify safe social engagement cues;
- Integrated somatic experiencing therapies for grounding exercises.
After 8 weeks, 70% of participants reported significant emotional shifts, per 2023 program outcome reports, enhancing long-term recovery adherence.
Evidence, Benefits, and Challenges
Polyvagal Theory’s evidence includes a 2021 meta-analysis in Frontiers in Psychology showing 55% improvement in PTSD symptoms via ventral activation, though implementation challenges persist in clinical models.
Integrating Polyvagal Theory yields key benefits, such as a 40% reduction in relapse rates and $5,000 annual savings per patient through targeted ventral vagal state activation, per ROI analyses from the American Psychological Association.
Stephen Porges’s more than 40 studies, plus Stephen Haines’s brain and nerve biology work in the book The Polyvagal Theory in Therapy, show that it works well to bring back signals of safety.
Challenges include therapist bias toward top-down cognitive approaches-addressed via 20-hour Polyvagal training programs-and client resistance in freeze states, mitigated by gentle somatic invitations like co-regulation exercises.
A Toronto clinic reported 60% healing rates by embedding these methods in group sessions.
Frequently Asked Questions
What does Polyvagal Theory mean in addiction treatment that addresses the whole person?
Addiction treatment for the whole person draws from Stephen Porges’ Polyvagal Theory. The theory covers how the autonomic nervous system shapes social behavior and emotional regulation. This builds a body-mind-spirit approach to end addiction. It focuses on restoring safety and connection by shifting from fight-flight-freeze states to ventral vagal calm, integrating therapy, mindfulness, and somatic practices.
How does polyvagal theory address trauma in addiction treatment that considers the whole person?
When applied to addiction treatment, Polyvagal Theory treats trauma as a disruption in the nervous system that often leads to addictive behaviors. Treatment emphasizes co-regulation through safe relationships, breathwork, and yoga to activate the ventral vagal system, helping individuals process trauma without re-triggering survival responses and fostering long-term recovery.
What role does the nervous system play in Polyvagal Theory in whole-person addiction treatment?
Polyvagal theory in addiction treatment describes three states of the autonomic nervous system-ventral vagal (safe and social), sympathetic (fight or flight), and dorsal vagal (shutdown)-and their links to addiction behaviors. Treatments that address the whole person identify and change these states through biofeedback, grounding exercises, and support from others. This creates strength to prevent relapse.
Does Polyvagal Theory help manage emotions in whole-person addiction treatment?
Polyvagal Theory used in whole-person addiction treatment aids emotional regulation. It lets people spot and settle autonomic nervous system responses through heart rate variability training and expressive arts therapy. This method lowers impulsivity and cravings by creating a feeling of safety, which helps people respond more evenly to stress during recovery.
What common methods from Polyvagal Theory are used in whole-person treatment for addiction?
In addiction treatment using Polyvagal Theory, people apply somatic experiencing, guided imagery, music therapy, and interpersonal neurobiology exercises. These methods activate the vagus nerve and repair social connections. These methods complement traditional addiction counseling by addressing the physiological roots of addiction holistically.
Does research support Polyvagal Theory in whole-person addiction treatment?
More research supports using Polyvagal Theory in addiction treatment that addresses the whole person. It works in care that accounts for trauma. Studies show it leads to better control of the nervous system and less substance use. We need more clinical trials, but brain science evidence shows its benefit in combined programs that treat the whole person for long-term recovery from addiction.






